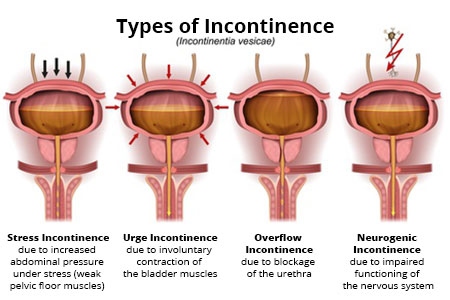
- Stress Incontinence: Involuntary urine leakage during activities that increase pressure on the bladder, such as coughing, sneezing, or laughing.
- Urge Incontinence: A sudden, intense urge to urinate followed by involuntary leakage, often caused by an overactive bladder.
- Overflow Incontinence: Constant dribbling of urine due to a bladder that doesn’t empty completely, often due to nerve damage or bladder blockage.
- Functional Incontinence: Inability to reach the bathroom in time due to physical or cognitive impairments, like arthritis or dementia.
Urinary Incontinence: Detailed Overview
Urinary incontinence (UI) is the loss of bladder control, leading to unintentional urine leakage. It is a common condition that affects people of all ages, but it is particularly prevalent in older adults, women, and those who have given birth. While UI is not a disease, it can significantly affect one’s quality of life and emotional well-being.
📊 Types of Urinary Incontinence
- Stress Incontinence
- Definition: Involuntary urine leakage due to physical stress on the bladder (e.g., coughing, sneezing, laughing, or lifting).
- Causes: Weakening of pelvic floor muscles, often due to pregnancy, childbirth, or aging.
- Common in: Women, particularly after childbirth or menopause.
- Urge Incontinence (Overactive Bladder)
- Definition: A sudden, intense urge to urinate followed by involuntary leakage.
- Causes: Overactivity of the bladder muscles, bladder infections, or neurological disorders.
- Common in: Older adults, especially those with diabetes, stroke, or multiple sclerosis.
- Overflow Incontinence
- Definition: Frequent dribbling of urine due to a full bladder that cannot empty completely.
- Causes: Blockage in the urinary tract, nerve damage, or weakened bladder muscles.
- Common in: Men with prostate issues, older individuals, or those with diabetes.
- Functional Incontinence
- Definition: Inability to reach the bathroom in time due to physical or cognitive impairments (e.g., arthritis, dementia).
- Causes: Mobility issues or cognitive decline.
- Common in: Older adults or individuals with mobility or cognitive disabilities.
- Mixed Incontinence
- Definition: A combination of stress and urge incontinence.
- Causes: Both weakened pelvic floor muscles and bladder overactivity.
- Common in: Older women and those who have given birth.
🧬 Causes of Urinary Incontinence
- Weak pelvic floor muscles (due to pregnancy, childbirth, or aging)
- Hormonal changes (e.g., menopause, which reduces estrogen and weakens pelvic tissues)
- Nerve damage from conditions like diabetes, stroke, Parkinson’s disease, or multiple sclerosis
- Prostate problems in men (enlarged prostate or prostate surgery)
- Bladder infections or irritation
- Medications (e.g., diuretics, sedatives)
- Obesity (extra weight can put pressure on the bladder)
- Chronic coughing (from conditions like smoking or asthma)
🔍 Symptoms of Urinary Incontinence
- Leakage of urine during physical activities like coughing, laughing, or sneezing (Stress Incontinence).
- Frequent, urgent need to urinate, sometimes with little warning (Urge Incontinence).
- Dribbling of urine when the bladder is overly full (Overflow Incontinence).
- Accidents due to inability to reach the bathroom in time (Functional Incontinence).
🩺 Diagnosis of Urinary Incontinence
- Physical examination: A pelvic exam in women to check for any signs of pelvic organ prolapse.
- Urinalysis: To rule out infections or blood in the urine.
- Bladder diary: A record of urination patterns, fluid intake, and leaks.
- Post-void residual test: Measures the amount of urine left in the bladder after urination (for overflow incontinence).
- Urodynamic testing: A set of tests to assess how well the bladder and urethra are storing and releasing urine.
- Cystoscopy: A procedure that allows doctors to look inside the bladder using a small camera.
💊 Treatment Options for Urinary Incontinence
🟢 Lifestyle Changes
- Fluid management: Adjusting fluid intake to avoid excessive amounts at night.
- Diet: Reducing caffeine, alcohol, and spicy foods that may irritate the bladder.
- Weight management: Reducing pressure on the bladder by losing weight.
🔵 Pelvic Floor Exercises (Kegels)
- Strengthening the pelvic floor muscles can help improve stress incontinence.
- Kegel exercises involve tightening and relaxing the pelvic floor muscles to improve bladder control.
🟠 Medications
- Anticholinergics: To relax the bladder and reduce urge incontinence.
- Alpha-blockers: For men with overflow incontinence due to prostate issues.
- Topical estrogen: To strengthen tissues in postmenopausal women.
🟡 Behavioral Therapies
- Bladder training: Gradually increasing the time between bathroom visits to retrain the bladder.
- Scheduled voiding: Going to the bathroom at regular intervals to prevent accidents.
🔴 Surgical Treatments
- Sling surgery: A common surgery for stress incontinence that supports the urethra.
- Prolapse surgery: To fix pelvic organ prolapse contributing to incontinence.
- Artificial sphincter: A device implanted to help control urine flow in severe cases of incontinence.
- Sacral nerve stimulation: A therapy that uses electrical impulses to control bladder function, especially for urge incontinence.
🟣 Devices
- Pessary: A device placed in the vagina to support the bladder and reduce leaks.
- Urethral inserts: Small devices worn inside the urethra to prevent leakage.
🌱 Natural Remedies and Lifestyle Adjustments
- Herbal supplements: Some herbs like horsetail or saw palmetto may help with bladder control.
- Acupuncture: May be used to stimulate nerves and improve bladder function.
- Biofeedback: A technique that helps individuals improve control over their bladder and pelvic muscles.
🧘♀️ Living with Urinary Incontinence
- Absorbent products (pads or underwear) for managing leaks.
- Counseling or support groups can be helpful for emotional and social support, as incontinence can lead to embarrassment and isolation.
- Social adjustments: Planning bathroom breaks during outings and knowing where restrooms are located can reduce anxiety.
🔄 Preventing Urinary Incontinence
While it may not be entirely preventable, you can reduce your risk by:
- Exercising pelvic muscles (Kegels).
- Maintaining a healthy weight.
- Avoiding heavy lifting.
- Treating chronic conditions, such as constipation or a chronic cough.
- Not smoking, which can weaken pelvic muscles due to chronic coughing.
Let me know if you’d like a visual diagram, tips on pelvic floor exercises, or further details on treatment options for urinary incontinence.

