- Minimally Invasive: Small incisions or no incisions; the hysteroscope is inserted through the vagina to treat uterine conditions like fibroids, polyps, and adhesions.
- Treatment: Used to remove growths, correct structural abnormalities, and treat abnormal bleeding, while preserving the uterus.
- Procedure: Performed under general or local anesthesia, with fluid used to distend the uterus for better visualization.
- Benefits: Short recovery (1-2 weeks), preserves fertility, minimal scarring, and quicker return to daily activities compared to traditional surgery.
Operative Hysteroscopy: Detailed Overview
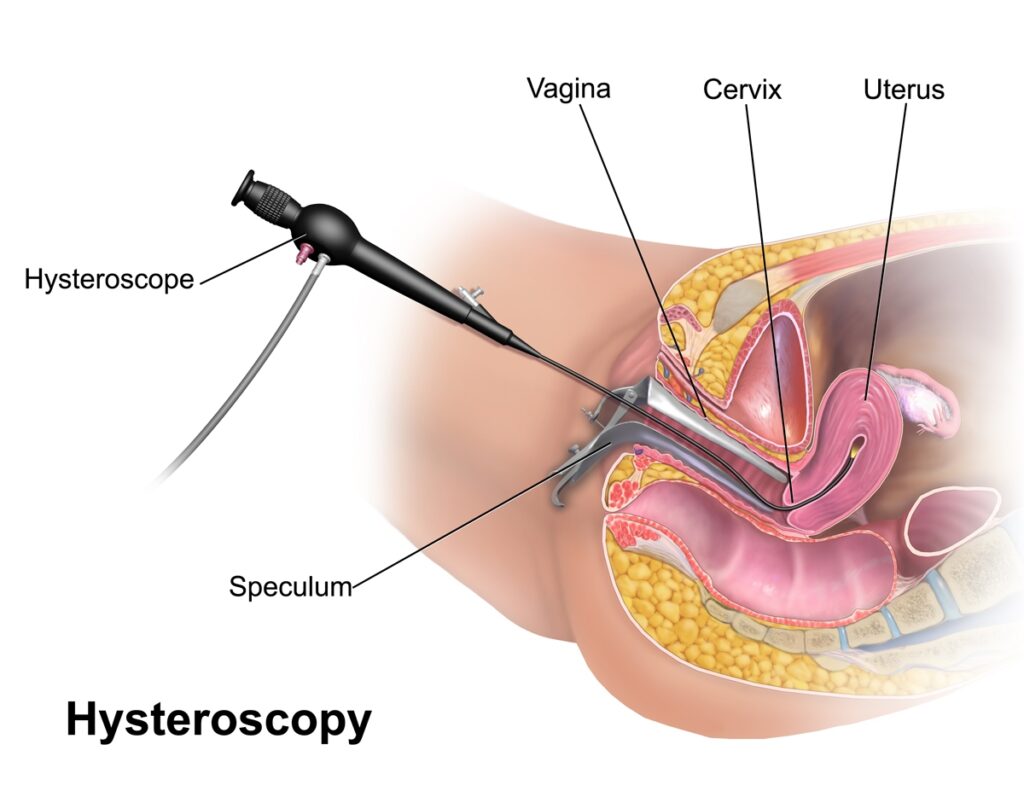
Operative hysteroscopy is a minimally invasive surgical procedure used to diagnose and treat various conditions of the uterus. This procedure is performed using a hysteroscope, a thin, flexible tube with a light and camera that allows the surgeon to visualize the inside of the uterus. It can also be used to treat problems such as fibroids, polyps, adhesions, and abnormal bleeding, without the need for large incisions.
🧬 What Is Hysteroscopy?
Hysteroscopy involves the use of a hysteroscope, which is inserted through the vagina and cervix into the uterus. A diagnostic hysteroscopy is used solely for diagnostic purposes, while an operative hysteroscopy involves both diagnosis and treatment of uterine issues. Operative hysteroscopy can be used to remove growths, correct structural abnormalities, and perform minor surgeries inside the uterus.
🏥 Conditions Treated with Operative Hysteroscopy
Operative hysteroscopy is often used to treat the following conditions:
- Uterine Fibroids: Non-cancerous growths in the uterus.
- Endometrial Polyps: Small growths attached to the lining of the uterus.
- Uterine Septum: A congenital abnormality where a dividing wall exists within the uterus.
- Asherman’s Syndrome (Intrauterine Adhesions): Scar tissue in the uterus that can result from previous surgeries or infections.
- Abnormal Uterine Bleeding: Excessive or irregular bleeding that cannot be explained by other means.
- Septate or T-shaped Uterus: Structural abnormalities affecting fertility.
- Retained Products of Conception: Tissue left in the uterus after a miscarriage or abortion.
🛠️ Procedure Steps for Operative Hysteroscopy
- Anesthesia: The procedure is usually performed under general anesthesia, but local anesthesia may be used for some procedures, depending on the case.
- Positioning: The patient is positioned in a stirrups position (similar to a pelvic exam).
- Insertion of the Hysteroscope: The hysteroscope, which is a thin tube with a light and camera, is inserted through the vagina and cervix into the uterus. The camera allows the surgeon to visualize the uterine cavity on a monitor.
- Distention of the Uterus: The uterus is typically filled with a sterile fluid or gas to expand it and create better visualization. This is important for accessing the uterine lining and any growths or abnormalities.
- Treatment:
- Resection or Removal of Fibroids/Polyps: Small surgical tools are passed through the hysteroscope to remove fibroids, polyps, or other abnormal growths.
- Correction of Septum or Adhesions: If the uterus is structurally abnormal, the surgeon may use surgical instruments to cut or remove the septum (the dividing wall) or adhesions.
- Electrosurgery: Sometimes, electrosurgical instruments are used to remove tissue or to treat bleeding areas.
- Closure: After the procedure, the instruments are removed, and any excess fluid is drained. The cervix may be sealed to prevent infections.
🕒 Duration and Recovery
- Surgery Duration: The procedure usually takes 30 minutes to 1 hour, depending on the complexity and the type of surgery being performed.
- Hospital Stay: It is typically an outpatient procedure, meaning patients can go home the same day.
- Recovery Time: Recovery time is generally quick:
- Mild cramping and spotting are common for 1-2 days after the procedure.
- Full recovery typically takes 1-2 weeks.
- Most women can return to normal activities within 2-3 days, though heavy lifting and strenuous activities should be avoided for a couple of weeks.
✅ Benefits of Operative Hysteroscopy
- Minimally invasive: Requires only small incisions or no incisions at all, reducing pain and scarring.
- Short recovery time: Most patients can resume regular activities quickly.
- Preserves fertility: Operative hysteroscopy allows surgeons to correct structural problems or remove growths while preserving the uterus, which is important for fertility.
- Quick diagnosis and treatment: Can be both diagnostic and therapeutic in a single procedure, often with minimal hospital stay.
- Lower risk of complications: Less blood loss and lower risk of infection compared to traditional open surgery.
⚠️ Risks and Complications
Though operative hysteroscopy is generally safe, it still carries some risks, including:
- Infection: There is a risk of infection in the uterus after the procedure.
- Bleeding: Some bleeding is normal, but excessive bleeding may require further intervention.
- Uterine Perforation: In rare cases, the hysteroscope may cause a tear or perforation in the uterine wall.
- Fluid Overload: If too much fluid is used during the procedure, it can lead to fluid overload and electrolyte imbalance.
- Scarring or Adhesions: In some cases, new adhesions may form after the surgery, which can lead to complications in future pregnancies.
- Injury to surrounding organs: Although rare, there is a slight risk of damaging nearby organs like the bladder or bowel.
🧪 Post-Operative Care
- Pain Management: Mild to moderate cramping and spotting are common for the first few days. Over-the-counter pain medications are usually sufficient.
- Activity: Patients are typically advised to avoid heavy lifting and strenuous exercise for 2 weeks to prevent complications.
- Follow-up: A follow-up appointment is usually scheduled 1-2 weeks after the procedure to check healing and address any concerns.
- Signs to Watch For: Contact your healthcare provider if you experience fever, excessive bleeding, or severe pain, as these could be signs of complications.
👶 Fertility After Operative Hysteroscopy
Operative hysteroscopy is often used to treat uterine abnormalities that affect fertility, such as fibroids, polyps, or adhesions. By removing or correcting these issues, the procedure can improve fertility. Most women can conceive naturally after the procedure, although some women may need to wait a few months for their uterus to fully heal.
❗ When Operative Hysteroscopy May Not Be Suitable
- Large or deeply embedded fibroids: These may be more suitable for removal through other methods, such as abdominal surgery.
- Extensive adhesions or structural issues: If the adhesions or uterine problems are widespread or severe, other surgical approaches might be required.
- Suspicion of uterine cancer: If a cancerous growth is suspected, a more extensive approach, such as a hysterectomy, may be necessary.
🧾 Conclusion
Operative hysteroscopy is a minimally invasive, effective, and low-risk treatment option for women dealing with uterine conditions like fibroids, polyps, and adhesions. It offers many advantages, including quick recovery, preservation of fertility, and lower risk of complications compared to traditional open surgery.

