- Squamous Cell Carcinoma – Most common type; linked to HPV or chronic irritation.
- Melanoma – Arises from pigment-producing cells; more aggressive.
- Adenocarcinoma – Develops in glandular tissue, like Bartholin’s glands.
- Basal Cell Carcinoma – Rare and slow-growing; usually less aggressive.
- Sarcoma – Very rare; originates in connective tissues of the vulva.
Vulvar Cancer: In-Depth Overview
Vulvar cancer is a rare type of cancer that occurs on the external female genitalia, primarily affecting the labia, but can also involve the clitoris, perineum, or vaginal opening. It typically develops slowly over years and is most common in older women, though it can affect younger women, especially those with certain risk factors like HPV.
🧬 Types of Vulvar Cancer
There are several types, with the most common being:
- Squamous Cell Carcinoma (~90%):
- Arises from the thin, flat cells lining the vulva.
- Often linked to HPV infection or chronic vulvar irritation (lichen sclerosus).
- Melanoma:
- Develops from pigment-producing cells (melanocytes).
- Less common, but more aggressive.
- Adenocarcinoma:
- Arises from glandular cells, often in the Bartholin’s glands.
- Basal Cell Carcinoma & Sarcoma:
- Rare; tends to grow slowly and spread less frequently.
⚠️ Signs and Symptoms
Early vulvar cancer may not cause obvious symptoms. Common signs include:
- Persistent itching or burning
- Pain or tenderness
- Thickened or discolored skin patches
- A lump, wart-like growth, or ulcer on the vulva
- Bleeding not related to menstruation
- Painful urination or intercourse
Any long-lasting vulvar irritation, lumps, or sores should be evaluated by a doctor.
🧪 Causes and Risk Factors
Major Risk Factors:
- HPV Infection (especially types 16 & 18)
- Age (most common in women over 60)
- Lichen Sclerosus – a chronic skin condition that causes thin, white patches on the vulva
- Smoking – weakens the immune system’s response to HPV
- Weakened immune system – from conditions like HIV or immunosuppressive therapy
- History of cervical or vaginal precancer or cancer
🔬 Diagnosis
- Physical Exam – Inspection of the vulva for abnormal areas.
- Biopsy – A small tissue sample is taken and examined for cancer cells.
- Colposcopy – A magnifying tool is used to examine the vulva closely.
- Imaging Tests – CT, MRI, or PET scans may be done to check for spread.
📊 Staging of Vulvar Cancer
- Stage I: Confined to the vulva or perineum.
- Stage II: Spread to adjacent tissues (e.g., lower urethra or vagina).
- Stage III: Spread to nearby lymph nodes.
- Stage IV: Spread to distant organs like the bladder, rectum, or beyond.
💉 Treatment Options
Treatment depends on cancer type, size, location, and stage, as well as overall health.
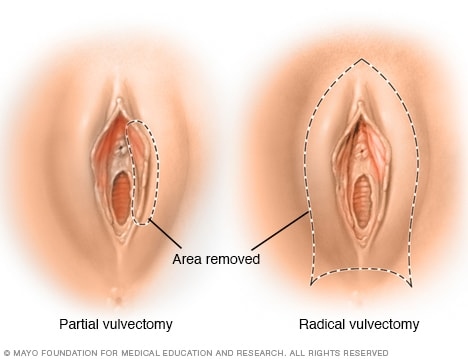
- Surgery (primary treatment):
- Wide local excision: Removes tumor and surrounding tissue.
- Vulvectomy: Partial or total removal of the vulva.
- Lymph node dissection: Removal of groin lymph nodes if cancer has spread.
- Radiation Therapy:
- Used before or after surgery, especially if lymph nodes are involved.
- Chemotherapy:
- Often combined with radiation in advanced cases or if surgery isn’t possible.
- Targeted Therapy / Immunotherapy:
- Newer options in clinical trials or for advanced, HPV-related cases.
🔄 Prognosis
- Early-stage vulvar cancer has a good prognosis with proper treatment.
- 5-year survival rate: Around 70–90% for localized cancer, but lower if it spreads to lymph nodes or distant organs.
🛡️ Prevention and Early Detection
- HPV Vaccination – Protects against high-risk HPV types.
- Regular gynecologic exams – Especially in women with risk factors.
- Quit smoking – Reduces the risk and improves immune defense.
- Monitor and treat vulvar conditions like lichen sclerosus.
- Prompt evaluation of any persistent itching, sores, or lumps.
✅ Conclusion
Vulvar cancer is uncommon but highly treatable if caught early. Awareness of symptoms and risk factors, regular pelvic exams, and HPV prevention are key to reducing risk and improving outcomes.

